Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Sensory Motor Multineuropathy Revealed A Schwannomatosis
*Corresponding author: Francesco B, Lucia F, Roberto A, Salvatore G, Giorgia B, Sensory Motor Multineuropathy Revealed A Schwannomatosis
Received: August 26, 2022; Published: September 16, 2022
DOI: 10.34297/AJBSR.2022.17.002314
Abstract
A 62-year-old man without significant anamnestic elements has been impossible to dorsiflexion of his right foot for about 2 years, without pain. Neurological and neurophysiological examination has identified a sensory motor multineuropathy. The particular pattern of involvement of the peripheral nervous system has oriented the magnetic resonance examination with evidence of multiple schwannomas and has allowed a first and fundamental differential diagnosis also orienting the choice of the optimal site for the biopsy examination. After performing the genetic examination as confirmation, positive for LZTR1, the patient undertook chemotherapy with clinical stability.
Keywords: Multineuropathy, Schwannomatosis, LZTR1
Introduction
Neurofibromatosis comprises a group of genetically distinct disorders of the nervous system, unified by the predisposition to develop tumors of the nerve sheaths. The three major forms of neurofibromatosis are: neurofibromatosis 1 (NF1), neurofibromatosis 2 (NF2) and schwannomatosis (NF3) [1]. The latter is a distinct clinical entity, of more recent identification and classification. It is characterized by multiple schwannomas in the absence of vestibular tumors. Patients with schwannomatosis account for 2-5% of those undergoing resection of schwannomas. Most cases are caused by the inactivation of pathogenic variants in SMARCB1 or LZTR1, tumor suppressor genes on chromosome 22 [2,3,5]. About a third of patients with schwannomatosis have tumors localized to a segment of the spine or a single limb. More frequent in the female sex with an average age between 25 and 60 years is characterized clinically by pain which is also the main indication for surgery; more rarely, hyposthenia and sensory deficits are observed. Magnetic resonance imaging (MRI) makes it possible to identify multiple, well-defined, rounded or oval lesions along the course of the peripheral nerves, at the level of the extremities. Lesions have low-intermediate signal strength in T1-weighted sequences and high in T2-weighted sequences. MRI makes it possible to exclude vestibular schwannomas, typical of NF2. The definitive diagnosis is histological. Surgical resection is decisive and associated with a good prognosis [1].
Introduction
C.P is a 52-year-old male patient suffering from progressive hyposthenia in the dorsiflexion of the right foot for about 2 years without lower back pain. It did not present any relevant anamnestic finds. In the outpatient clinic, the neurological evaluation documented a paralysis of the right popliteo-external sciatic nerve associated with a mild hyposthenia of the left ileopsoas muscle. No deficits of superficial sensibility were found, but to profound sensibility with hypopallesthesia to the external malleolus of the left. Electromyography revealed diffuse sensory motor multineuropathy with chronic neurogenic damage. No findings such as fibrillation or PSW in the lower limbs but only during exertion single oscillation framework of the MUP with accelerated recruitment frequency was founded in biceps femoris muscle, long peroneal muscle, anterior tibial and extensor hallucis longus muscle on the right and long peroneal and extensor hallucis longus muscle on the left. In the upper limbs, a chronic neurogenic suffering of the first dorsal interrosseous and left brachial biceps was evident.
Also, in this district do not signs of muscle irritation was evident. In view of these “leopard spot” findings identifying a multineuropathy rather than a polyneuropathy was then carried a complete blood test of first and second level including blood count, thyroid hormones, TSH, dosage of vitamin B12, erythrocyte sedimentation rate, C-reactive protein, ANA, ENA, glycated hemoglobin, fasting blood glucose, liver and kidney function indices and antibody assay against onconeural antigens which were all negative. A lumbar puncture was also carried out, negative. For the involvement of the right biceps femoral muscle, in addition to an MRI of the brain and lumbosacral marrow, a bilateral magnetic resonance imaging of the thigh was also performed, with evidence of multiple schwannomas, of which the largest one present along the right L5 root territory in the context of m. psoas (figure one, panel A). These findings did not affect the vestibular nerves (figure one, panel D).
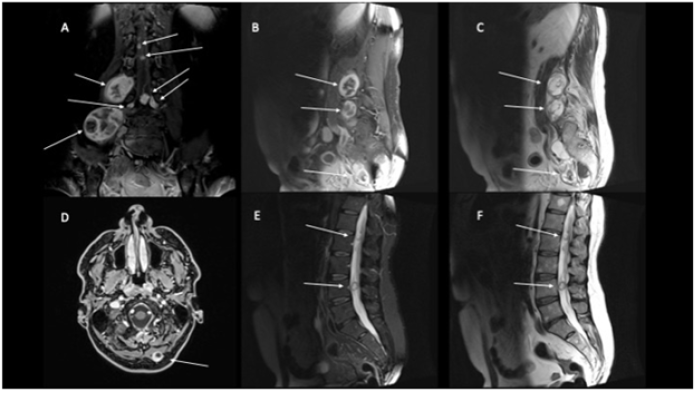
Figure 1: Brain, Rachis and Thigh MRI show multiple parenchymatous formations with a heterogeneous structure in the context of the muscle belly of the psoas, extending up to the ileus muscle and to the right lateral side of the L4 and L5 vertebrae. Findings with the same characteristics in correspondence were found at paraspinous nerve roots from L3 to L5, cauda and at the right paramedian occipital region (white arrow). T1 hyperintense components indicating hemorrhage or fatty degeneration occurs in a small fraction. Same lesions show T2 hyperintense, because cystic degeneration is common, and T1 with gadolinium showing marked and non-homogeneous contrast enhancement. Unlike neurofibromas, which tend to grow centrally from a nerve, schwannomas more frequently tend to have eccentric growth [1].
Given the diagnostic suspicion of a probable schwannomatosis, a neurosurgical evaluation was carried out, which placed an indication on biopsy of the larger neoformation, present in the context of the right psoas. After the biopsy, “fused cells” were documented, associated with isolated atypical epithelioid cells, positive for the immunophenotype S100 +, SOX10+, panCK-, Actin smooth muscle-, desmin -, HMB45-, Melan A-, CD34-. Mitosis is not observed. Ki67 less than 1%”. This finding was found to be compatible with the diagnosis of Schwannomatosis. After total body PET/CT, which was negative, the patient also underwent a genetic test that detected a germline mutation positive for LZTR1. He is currently being treated with Bortezomib and appears stable.
Discussion
When multiple schwannomas are observed, the main differential diagnosis is neurofibromatosis type 2 [2]. It is essential to carry it out, since the management of the patient and family members changes between the two different pathologies. First, the anamnesis is crucial as in the context of NF2 a family history of vestibular schwannomas, hearing loss, tinnitus or ependymomas is possible. Therefore, the main feature that distinguishes NF2 from schwannomatosis is the presence of bilateral vestibular schwannomas on MRI examination of the brain, which are a main clinical feature of NF2 especially if the patient is over 30 years of age, which are completely incompatible with a diagnosis of schwannomatosis. From a radiological point of view, it is important to remember that unlike neurofibromas, which tend to grow centrally from a nerve, schwannomas tend more frequently to have eccentric growth [2].
However, mosaic forms of NF2 (about 30% of all people with NF2) may have multiple schwannomas and no vestibular schwannoma, thus mimicking the presentation of schwannomatosis [4]. In one study, the NF2 mosaic misdiagnosed as schwannomatosis accounted for at least 9% of clinically diagnosed schwannomatosis cases [5]. Therefore, it becomes important to make a genetic confirmation diagnosis. The genes currently known to be involved in schwannomatosis are SMARCB1 and LZTR1. In the phenotype associated with LRZT1, the development of unilateral vestibular schwannomas is sometimes possible, thus imitating the presentation of NF2 [5,6]. Another help in making the differential diagnosis comes to us from pathological anatomy. In the case of the patient a strong expression of the S100 protein, no mitosis and positive markers such as SOX10 [3] can be associated with both neurofibromatosis and schwannomatosis, but in view of the lack of involvement of the cranial nerves at the MRI examination [2], the definitive confirmation came to us with the positive genetic examination for LRZT1 [4].
Conclusion
In the case of multineuropathies, even if not painful, it is important to orient the type of imaging through a neurological examination completed by a neurophysiological examination such as electromyography. The choice of the type of imaging, MRI, and the location where to perform it is in fact a key moment in the diagnostic path. In the case of Schwhannomatosis it is essential to identify schwannomas, in their extension and location, both for a differential diagnosis with NF2 and to be able to perform a diagnostic biopsy.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Mac Collin M, Woodfin W, Kronn D, Short MP (1996) Schwannomatosis: a clinical and pathologic study. Neurology 46: 1072-1079.
- Koontz NA (2013) Schwannomatosis: the overlooked neurofibromatosis? AJR Am J Roentgenol. 200(6): W646-W653.
- Pekmezci M, David E Reuss, Angela C Hirbe, Sonika Dahiya, David H Gutmann, et al. (2015) Morphologic and immunohistochemical features of malignant peripheral nerve sheath tumors and cellular schwannomas. Mod Pathol 28(2): 187-200.
- Miriam J Smith, Naomi L Bowers, Michael Bulman, Carolyn Gokhale, Andrew J Wallace, et al. (2017) Revisiting neurofibromatosis type 2 diagnostic criteria to exclude LZTR1-related schwannomatosis Neurology 88(1): 87-92.
- Kehrer-Sawatzki H, Lan Kluwe, Reinhard E Friedrich, Anna Summerer , Eleonora Schäfer, et al. (2018) Phenotypic and genotypic overlap between mosaic NF2 and schwannomatosis in patients with multiple non-intradermal schwannomas. Hum Genet 137(6-7): 543-552.
- Evans DG, Naomi L Bowers, Simon Tobi, Claire Hartley, Andrew J Wallace, et al. (2018) Schwannomatosis: a genetic and epidemiological study. J Neurol Neurosurg Psychiatry 89(11): 1215-1219.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.